Journal of Radiology and Imaging
An International Peer-Reviewed Open Access Journal
ISSN 2399-8172


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Radiology and Imaging
Volume 5, Issue 1, January 2021, Pages 1–4
Original researchOpen Access
Scattered radiation during osteosynthesis of the distal radius: A phantom study
-
Legerstee IWF1,*
 , Oosterveer TTM2, Molenaar MA2, Rasenberg DWM3, Spoon EQW4, Verhoeven VWJ5 and
Elst M van der6, 7
, Oosterveer TTM2, Molenaar MA2, Rasenberg DWM3, Spoon EQW4, Verhoeven VWJ5 and
Elst M van der6, 7
- 1 Leiden University Medical Center, The Netherlands
- 2 Technical Medicine, Delft University of Technology; Erasmus University Medical Center; Leiden University Medical Center, The Netherlands
- 3 Department of Biomedical Engineering, Delft University of Technology, The Netherlands
- 4 Reinier de Graaf Hospital, Delft, The Netherlands
- 5 Department of Medical Physics, Reinier de Graaf Hospital, Delft, The Netherlands
- 6 Department of Surgery and Trauma, Reinier de Graaf Hospital, Delft, The Netherlands
- 7 Faculty of Mechanical, Maritime and Materials Engineering, Delft University of Technology, The Netherlands
*Corresponding author: Ingmar Legerstee, Medical student, Leiden University Medical Center, Leiden, The Netherlands. Rochussenstraat 307B, Rotterdam, 3023DG, The Netherlands. Tel.: +316 10340576; Email: I.W.F.Legerstee@umail.leidenuniv.nl
Received 30 September 2020 Revised 28 November 2020 Accepted 10 December 2020 Published 19 December 2020
DOI: http://dx.doi.org/10.14312/2399-8172.2021-1
Copyright: © 2021 Legerstee IWF, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Modern fracture surgery requires an increasing number of operative procedures utilising radiological control. During osteosyntheses patients receive scattered radiation when fluoroscopy is used. Unlike operating-room staff, patients are not protected during these procedures. The aim of this study was to measure the amount of scattered radiation in the phantom plane during a simulated osteosynthesis in order to evaluate the patient’s need for protection. A lower arm anthropomorphic phantom was irradiated with the use of a Philips BV Pulsera C-arm. The amounts of scattered radiation at distances from 10 to 160 cm and angles of 0 to 180 degrees in the phantom plane were measured with a real-time dosimeter. The same amount of measurements was repeated with a fixation plate on top of the phantom to simulate a fracture reduction operation. The maximum amount of scattered radiation was 1.63 µSv at a distance of 10 cm from the edge of the radiation beam. This phantom study shows that scattered radiation during osteosyntheses of the distal radius is negligible and therefore no patient protection is needed. The results should be interpreted carefully as this is a phantom study.
Keywords: scattered radiation; radiation dosage; C-arm; fluoroscopy; distal radius
IntroductionTop
Correct fracture and implant positioning is checked during surgery using fluoroscopy. The C-arm is the most common fluoroscopic modality. Besides the primary radiation, which is used to generate the x-ray image, patients are also exposed to scattered (secondary) radiation, which delivers a dose to the patient, but does not contribute to the x-ray image. Scattered radiation is radiation that changes direction through the interaction of the x-ray beam and encountered human tissue and objects such as the operation table [1]. Medical staff are protected during various surgical procedures from radiation by lead aprons, lead collars and lead glasses. Patients, however, are not protected against this radiation. The amount of scattered radiation medical staff receive during fluoroscopy has been thoroughly investigated in several studies [2-4]. However, minimal literature is available about scattered radiation doses absorbed by patients. The primary endpoint of this phantom study was to measure the amount of scattered radiation in the phantom plane during a simulated osteosynthesis in order to evaluate the patient’s need for protection.
Materials and methodsTop
A common performed operation is a distal radius fracture reduction. To simulate a distal radius fracture reduction, an anthropomorphic phantom of the lower arm was placed in a supinated position on the operation table (Figure 1). This phantom was irradiated by the Philips BV Pulsera Vision C-arm (Figure 2). This is a mobile fluoroscopy system. The anthropomorphic phantom consisted of a cadaver bone surrounded by polydimethylsiloxane (PDMS) with a density close to the density of human soft tissue [5]. Tube voltage was set at 50 kV, which is a usual setting during fluoroscopy at Reinier de Graaf Hospital in Delft. Consequently, the C-arm calculated a tube current of 0.22 mA. The product of the current and time was 13.2 mAs. The phantom was irradiated for 60 seconds for each measurement. This amount of time was chosen due to the fact that most orthopaedic surgeries requiring fluoroscopy do not need more than 60 seconds of screening time. Spoon et al. showed that the average screening time for hand or wrist surgery was 38 seconds [6]. The Berthold LB126 dose rate monitor was used for scatter radiation measurements. The measurements were done at different angles in degrees (0, 22.5, 45, 67.5, 90, 112.5, 135, 157.5, 180) and distances in centimeters (10, 20, 40, 80, 100, 120, 140, 160) from the edge of the radiation beam in the phantom plane (Figure 2). For the measurements at 0 degrees, the C-arm was moved 45 degrees relative to the phantom as is indicated in Figure 2. The radiation beam had a diameter of 13.5 cm at a height of 38.5 cm from the radiation source.

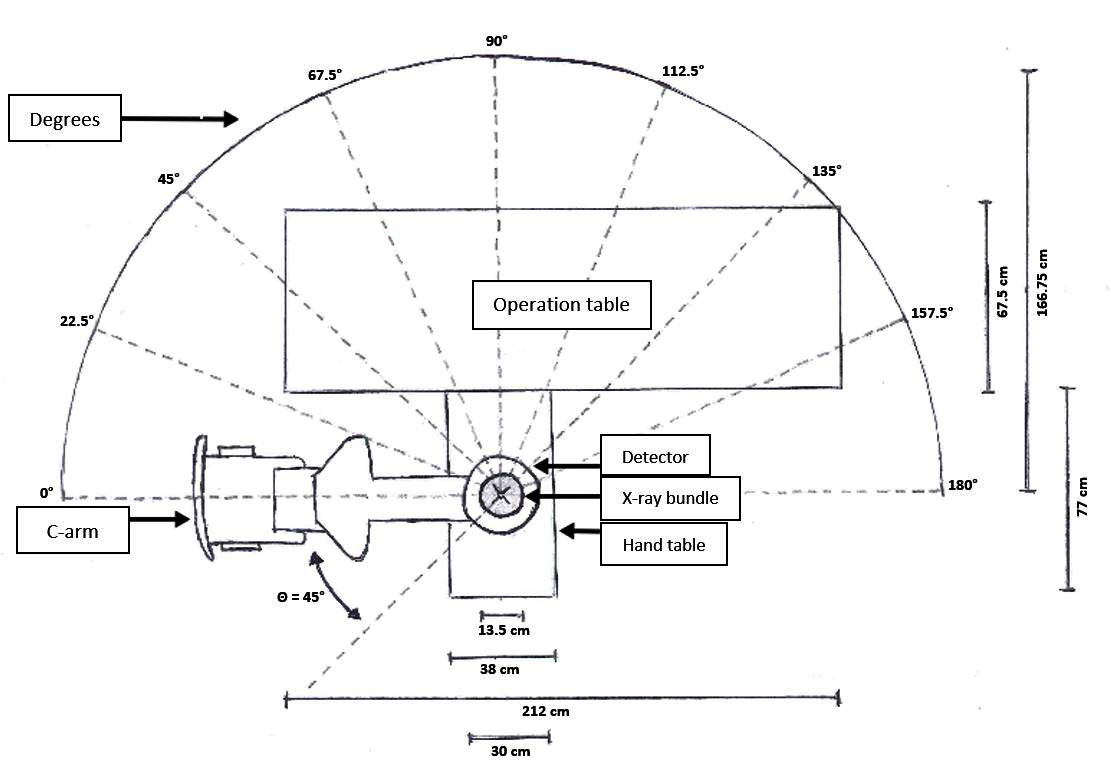
The net amount of scattered radiation was calculated by subtracting the average background radiation per 60 seconds. The background radiation was measured by placing the dosimeter in the operation theatre. To evaluate the impact of an osteosynthesis plate on the amount of scattered radiation, the actions described above were repeated with an osteosynthesis plate on top of the phantom. After each measurement the amount of scattered radiation, the time of irradiation, the dose area product (DAP) value and the cumulative dose were noted. The scattered radiation measurements were averaged for each distance.
Data analysis
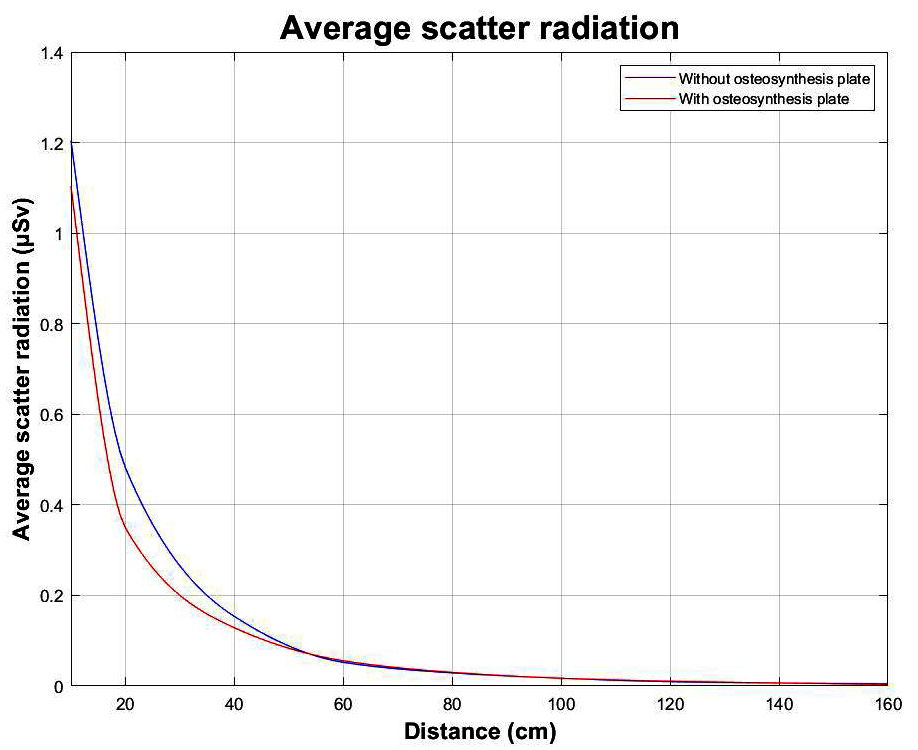
In order to visualise the average scattered radiation, a line graph was plotted using Matlab (version 2017a).
ResultsTop
The maximum amount of scattered radiation with and without the osteosynthesis plate was 1.63 µSv from the edge of the radiation beam at a distance of 10 cm and an angle of 0 degrees. For all distances, the average scattered radiation doses were lower than or equal to 1.20 µSv.
The equivalent dose received by the phantom after 60 seconds was 125 µSv. The average amount of background radiation after 60 seconds was 0.0020 µSv. Table 1 and 2 show the amounts of scattered radiation, corrected for the background radiation, with and without the osteosynthesis plate after 60 seconds, respectively. In addition, both tables show the average amount of scattered radiation per distance.
| 10 cm | 20 cm | 40 cm | 60 cm | 80 cm | 100 cm | 120 cm | 140 cm | 160 cm | |
| 0° | 1,58 | 0,36 | 0,15 | 0,08 | 0,05 | 0,03 | 0,02 | 0,02 | 0,02 |
| 22.5° | 1,48 | 0,63 | 0,20 | 0,07 | 0,04 | 0,04 | 0,02 | 0,02 | 0,01 |
| 45° | 1,54 | 0,54 | 0,20 | 0,08 | 0,04 | 0,02 | 0,02 | 0,01 | 0,01 |
| 67.5° | 1,03 | 0,48 | 0,16 | 0,04 | 0,01 | 0,01 | 0,01 | 0,00 | 0,00 |
| 90° | 0,22 | 0,29 | 0,11 | 0,01 | 0,01 | 0,00 | 0,00 | 0,00 | 0,00 |
| 112.5° | 1,09 | 0,45 | 0,15 | 0,04 | 0,01 | 0,01 | 0,00 | 0,00 | 0,00 |
| 135° | 1,26 | 0,49 | 0,16 | 0,06 | 0,03 | 0,01 | 0,01 | 0,00 | 0,00 |
| 157.5° | 1,37 | 0,57 | 0,14 | 0,06 | 0,04 | 0,02 | 0,01 | 0,01 | 0,00 |
| 180° | 1,29 | 0,59 | 0,14 | 0,05 | 0,05 | 0,03 | 0,01 | 0,01 | 0,01 |
| Average (SD) | 1,20 (±0,39) | 0,49 (±0,10) | 0,15 (±0,027) | 0,05 (±0,021) | 0,03 (±0,016) | 0,02 (±0,012) | 0,01 (±0,0074) | 0,01 (±0,0079) | 0,00 (±0,0068) |
| 10 cm | 20 cm | 40 cm | 60 cm | 80 cm | 100 cm | 120 cm | 140 cm | 160 cm | |
| 0° | 1,63 | 0,34 | 0,14 | 0,08 | 0,05 | 0,03 | 0,02 | 0,02 | 0,01 |
| 22.5° | 1,62 | 0,36 | 0,15 | 0,08 | 0,05 | 0,03 | 0,02 | 0,02 | 0,01 |
| 45° | 1,23 | 0,26 | 0,12 | 0,05 | 0,03 | 0,02 | 0,01 | 0,01 | 0,01 |
| 67.5° | 0,92 | 0,43 | 0,14 | 0,03 | 0,02 | 0,01 | 0,01 | 0,00 | 0,00 |
| 90° | 0,21 | 0,25 | 0,10 | 0,03 | 0,01 | 0,01 | 0,00 | 0,00 | 0,00 |
| 112.5° | 0,78 | 0,36 | 0,12 | 0,04 | 0,01 | 0,00 | 0,00 | 0,00 | 0,00 |
| 135° | 1,16 | 0,22 | 0,09 | 0,05 | 0,02 | 0,01 | 0,01 | 0,00 | 0,00 |
| 157.5° | 1,06 | 0,42 | 0,15 | 0,08 | 0,05 | 0,03 | 0,02 | 0,01 | 0,00 |
| 180° | 1,44 | 0,54 | 0,17 | 0,08 | 0,05 | 0,03 | 0,02 | 0,01 | 0,01 |
| Average (SD) | 1,11 (±0,42) | 0,35 (±0,096) | 0,13 (±0,024) | 0,06 (±0,021) | 0,03 (±0,017) | 0,02 (±0,011) | 0,01 (±0,0079) | 0,01 (±0,0079) | 0,00 (±0,0050) |
Figure 3 shows two line graphs of the average amount of scattered radiation at the different distances.
Since the settings of the C-arm (tube current and tube voltage) were kept constant and the time of fluoroscopy was 60 seconds for every measurement, the average DAP value for the measurements without the osteosynthesis plate was 0.0286 Gy * cm2 and 0.0281 Gy * cm2 for the measurements with the osteosynthesis plate.
DiscussionTop
In this phantom study the maximum amount of scattered radiation was 1.63 µSv. For all distances, the average scattered radiation doses were lower than or equal to 1.20 µSv. In Figure 3 one can notice that the average amount of scattered radiation approximately behaves according to the inverse-square law [7].
At 10 cm away from the radiation beam and at an angle of 90 degrees the measured amounts of scattered radiation were lower than the measured amounts of scattered radiation at 20 cm and an angle of 90 degrees. The reason for this contradiction is probably because the dosimeter was placed directly against the phantom. Possibly, the dosimeter was shielded off by the phantom.
In general, the amounts of scattered radiation were lower at the angles of 67.5, 90 and 112.5 degrees for all distances. This could be explained by the shape of the phantom which distributes the scattered radiation in different directions. A second explanation could be the presence of more phantom material in the 90 degrees direction which partly absorbs the scattered radiation.
Amounts of scattered radiation during simulated C-arm procedures have been reported by other studies. Giordano et al. performed scattered radiation measurements on different heights relative to an arm phantom and used multiple dosimeter badges [1, 8]. We purposely chose to measure the scattered radiation on the same level as the phantom. The used method simulates where the patient normally would receive the scattered radiation. Singer et al. (2011) measured the scattered radiation at 2.54 cm from the image intensifier in the phantom plane on a wrist and on an elbow phantom [9]. The amount of scattered radiation that was found in this study was 8.64×10-4 millisievert per second (mSv/s). Moreover, Singer et al. (2005) measured the scattered radiation in the phantom plane using a wrist phantom. The maximum amount of scattered radiation that was found in this study was 0.569 mSv/s at a distance of 0 cm from the image intensifier.
Several potential limitations of this study should be addressed. In this research one type of C-arm was used, namely the Philips BV Pulsera. Other C-arms may not show the same scattered radiation pattern as the Philips BV Pulsera. This is because of the fact that different manufacturers use different x-ray tubes and therefore the x-ray spectrum will be different between the C-arms of these manufacturers. This will also give different scatter radiation patterns. Furthermore, only one type of dosimeter was used, the Berthold LB126. This dosimeter is quite large which means it averages the scattered radiation over a large volume. Because of this the position of the different measurements is somewhat less accurate. Also, a cadavaric bone surrounded by silicone was used as a phantom. The material, more or less, has the same density as a human wrist [5]. Still the ratio of soft tissue to bone of the phantom is not the same as the ratio of soft tissue to bone of a human wrist. At last, a ‘Stryker 1001 Emergency Care Stretcher’ was used. This is not an operation table that is used in daily practice. This means there is a chance that this table has influenced the pattern of scattered radiation.
Scattered radiation may contribute to a high effective dose on radiation sensitive tissues, such as the thyroid gland and gonads. Spoon et al. (2019) recently measured scattered radiation doses at the thyroid gland, breast tissue, and gonads in 205 patients undergoing primary osteosyntheses of acute fractures of hand/wrist, shoulder, ankle, knee and hip. The highest median effective dose was 60.43 µSv (IQR 33.84-100.76) at the gonads during hip osteosynthesis. The highest median fluoroscopy time was 59 seconds (IQR 48-115). According to IRCP recommendations, no deterministic effects are expected below a short term radiation dose of 100 millisievert (Sv) [10]. Therefore the amount of scattered radiation during osteosynthesis does not seem to significantly increase the risk of cancer [11]. This research aimed to measure the scattered radiation during a simulated C-arm guided orthopedic procedure to confirm the findings by Spoon et al.
ConclusionTop
If someone received an equivalent dose of 100 mSv at once, this would increase the lifetime risk of developing cancer by 0.8 percent [11]. The maximum amount of scattered radiation in this research is 105 times lower than 100 mSv. Based on the results of this phantom study, the increased chance of developing cancer will be minimal. This implicates that protection of the patient during osteosyntheses of the distal radius is not needed. This recommendation should be interpreted with caution as this is a phantom study.
Conflicts of interest
Authors declare no conflict of interest.
ReferencesTop
[1]Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-c-arm fluoroscopy. J Bone Joint Surg Am. 2007; 89(5):948–952.Article Pubmed
[2]Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005; 13(1):69–76.Article Pubmed
[3]Mahajan A, Samuel S, Saran AK, Mahajan MK, Mam MK. Occupational radiation exposure from C arm fluoroscopy during common orthopaedic surgical procedures and its prevention. J Clin Diagn Res. 2015; 9(3):Rc01–4.Article Pubmed
[4]Alonso JA, Shaw DL, Maxwell A, McGill GP, Hart GC. Scattered radiation during fixation of hip fractures. Is distance alone enough protection? J Bone Joint Surg Br. 2001; 83(6):815–818.Article Pubmed
[5]White DR, Griffith RV, Wilson IJ. Report 46. Journal of the International Commission on Radiation Units and Measurements. 2016; os24(1):NP.Article
[6]Spoon EQW, Van Lieshout EMM, Wijffels MME, Verhoeven VW, Van der Elst M. The effective dose due to scattered radiation at patients during primary osteosynthesis; a multicenter prospective observational study. Injury. 2019; 5(5):1172–1176.Article Pubmed
[7]van den Eijnde J, Schouwenburg M. Praktische Stralingshygiëne. Utrecht: Syntax Media; 2013. 136.
[8]Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR, 2nd. Patient and surgeon radiation exposure: comparison of standard and mini-C-arm fluoroscopy. J Bone Joint Surg Am. 2009; 91(2):297–304.Article Pubmed
[9]Singer G, Herron B, Herron D. Exposure from the large C-arm versus the mini C-arm using hand/wrist and elbow phantoms. J Hand Surg Am. 2011; 36(4):628–631.Article Pubmed
[10]The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37(2-4):1–332. Available from:https://www.icrp.org/publication.asp?id=ICRP%20Publication%20103
[11]Verdun FR, Bochud F, Gundinchet F, Aroua A, Schnyder P, et al. Quality initiatives radiation risk: what you should know to tell your patient. Radiographics. 2008; 28(7):1807–1816.Article Pubmed


