Journal of Modern Human Pathology
An International Peer-Reviewed Open Access Journal
ISSN 2397-6845


- Download PDF
- |
- Download Citation
- |
- Email a Colleague
- |
- Share:
-
- Tweet
-

Journal of Modern Human Pathology
Volume 1, Issue 5, September 2016, Pages 39–43
Original researchOpen Access
Analytic turnaround time study for integrated reporting of pathology results on electronic medical records using the Illuminate system
- 1 Department of Pathology and Laboratory Medicine, Kansas University Medical Center, Kansas City, Kansas 66160, USA
*Corresponding author: Ossama Tawfik, MD, PhD, Professor, Department of Pathology and Laboratory Medicine, Kansas University Medical Center, 3901 Rainbow Boulevard, Kansas City, Kansas 66160, USA. Tel.: (913) 588-1185; Fax: (913) 588-8780; E-mail: otawfik@kumc.edu
Received 30 June 2016 Revised 05 August 2016 Accepted 16 August 2016 Published 25 August 2016
DOI: http://dx.doi.org/10.14312/2397-6845.2016-7
Copyright: © 2016 Tawfik O, et al. Published by NobleResearch Publishers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
AbstractTop
Timely pathology results are critical for appropriate diagnosis and management of patients. Yet workflows in laboratories remain ad hoc and involve accessing multiple systems with no direct linkage between patient history and prior or pending pathology records for the case being analyzed. A major hindrance in timely reporting of pathology results is the need to incorporate/interface with multiple electronic health records (EHRs). We evaluated the Illuminate PatientView software (Illuminate) integration into pathologist's workflow. Illuminate is a search engine architecture that has a repository of textual information from many hospital systems. Our goal was to develop a comprehensive, user friendly patient summary display to integrate the current fractionated subspecialty specific systems. An analytical time study noting changes in turnaround time (TAT) before and after Illuminate implementation was recorded for reviewers, including pathologists, residents and fellows. Reviewers' TAT for 359 cases was recorded (200 cases before and 159 after implementation). The impact of implementing Illuminate on transcriptionists’ workflow was also studied. Average TAT to retrieve EHRs prior to Illuminate was 5:32 min (range 1:35-10:50). That time was significantly reduced to 35 seconds (range 10 sec-1:10 min) using Illuminate. Reviewers were very pleased with the ease in accessing information and in eliminating the draft paper documents of the pathology reports, eliminating up to 65 min/day (25-65 min) by transcriptionists matching requisition with paperwork. Utilizing Illuminate improved workflow, decreased TAT and minimized cost. Patient care can be improved through a comprehensive patient management system that facilitates communications between isolated information systems.
Keywords: illuminate; turnaround time; workflow; anatomic pathology; integrated reporting; electronic medical records
IntroductionTop
While the implementation of electronic health records (EHRs) is increasing throughout the country, very little is publicized about their impact on clinical practices in pathology laboratories. With the advent of the Centers for Medicaid & Medicare Services (CMS) Electronic Health Records Incentive Program, laboratories are faced with an unprecedented need to establish and maintain interfaces to multiple different systems. The sole interface or connection between laboratory information systems (LIS) to the hospital information system (HIS) becomes insufficient. Anatomic pathology systems also have to interface their reports to the EHRs. Hospital and laboratory information technology (IT) departments are tasked with the challenge of interfacing many custom systems for individual subspecialties [1-5].
To establish functionally efficient connectivity with EHRs, laboratories have two choices: either purchase or design specific robust interfaces linking the different areas of the LIS directly to EHRs or use an intermediary third-party vendor as the "middleman" to disseminate back and forth information between LIS and EHRs in realtime. Technical, capital and personnel resources are needed to maintain such systems. With the enormous technological advances, the opportunity has emerged to develop integrated systems to meet these new mandates.
Timely pathology results are critical for appropriate diagnosis and management of patients. A major hindrance in timely reporting of pathology results is the need to incorporate multiple EHRs and user interfaces, each of which often requires multiple logins throughout the day each using often unique usernames and passwords [6-9]. Unfortunately, most if not all anatomic pathology system remain ad hoc to LIS and HIS with no direct linkage to the multitude of EHR systems for the accession of patients' medical records and prior or pending pathology records for the case being analyzed. Isolation of data systems causes unnecessary delay in the pathologists' workflows and can be detrimental to the quality and outcomes of patient care. These detrimental effects underscore the need for innovative workflow integration across multiple systems that facilitate the synthesis and dissemination of data produced by the different specialties.
In this study we investigated the impact of a point of interpretation dynamic patient summary software which has been well established in radiology workflows in surgical pathology laboratories. We compared times to access necessary information from our EPIC EMR (Verona, WI) and LIS with and without the integration of the Illuminate PatientView software (Softek Solutions, Inc., Kansas City, KS) with our anatomic pathology information system (CoPath, Sunquest, Tucson, AZ). This software architecture is inverted search engine, developed eight years ago for driving radiology research across the entire patient enterprise. The index allows sub-second access to all text and data fields of reports and clinical documents in the Radiology Information System, LIS and EHRs. In fact, radiologists at our institution and across the nation have successfully been using the search system for years with outstanding results. The PatientView module of the system builds on this platform by focusing on an individual patient's records, driven by synchronizing on the medical record number context of the primary system. This instant access to relevant patient history and results of prior procedures is essential to achieving the lean concept of "first time quality" making better-informed decisions in less time. Our ultimate goal is to develop a comprehensive, user friendly integrated electronic patient summary utilizing this software to achieve meaningful interoperability.
Patients and methodsTop
At the University of Kansas Hospital, Illuminate PatientView software was incorporated into the workflow of the sign out operation for surgical pathology samples. Following a period of testing and validation to adapt the PatientView module to include all the necessary clinical, radiological, pathology and clinical laboratory information required by pathologists for an expedited, accurate, complete and simple sign out process, the system was introduced for departmental evaluation by residents, fellows and staff pathologists in the study. Before implementation accuracy of transfer of all information between CoPath and the Illuminate server was performed. Validation checks were done on 10% of the documents from each year, 2007 to 2013 as required by national and institutional standards. All electronically archived cytology, surgical pathology, flow cytometry and autopsy reports for all samples were transferred and retrieved by the Illuminate system with a 100% success rate. Briefly, test software was installed on one workstation connecting CoPath with Illuminate to simultaneously open sampled reports in CoPath and Illuminate. Reports were randomly selected by the laboratory IT team. These reports were then compared for completion and accuracy. Validation studies performed on about 1000 randomly selected reports from 2007 to 2013 were performed as required by national and institutional standards. Validation studies were not performed on reports prior to 2008 as that was the year when the hospital started the electronic medical archival operation. Validated reports included gynecologic and non-gynecologic cytologic reports, fine needle aspiration, flow cytometry, surgical pathology and outside consultation reports. All electronically archived cytology, surgical pathology, flow autopsy reports for all samples were transferred and retrieved by Illuminate without problems throughout the duration of the study.
Formalized training of residents, fellows, pathologists and supporting laboratory personnel began four weeks prior to implementation. Each user was offered personalized training at their workstation whenever needed. A second monitor was installed at each of the users' workstation to improve their experience while reporting their findings on one monitor and simultaneously reviewing other medical records in Illuminate on the other monitor. In addition, during the implementation, there was full time support by the laboratory and the Softek company information systems staff.
A time study recording TAT and pathologists' satisfaction with the Illuminate software and its impact on the transcriptionists’ workflow was performed. The TAT before and after Illuminate implementation was recorded for seven reviewers. Random selections of reviewers with varied experience were selected including pathologists, residents and fellows to participate in the study to avoid bias in data analysis. The reviewed cases prior to and after implementation of Illuminate were of similar complexity. Fifteen to twenty cases were recorded per reviewer both prior and after implementation. Reviewers’ TAT for 359 cases was recorded, including 200 cases prior and 159 post implementation. For each reviewer, time was recorded from the time the case is accessed in CoPath for microscopic evaluation until the rendition of final diagnoses by pathologists or preliminary diagnoses by residents and fellows.
Components of the before Illuminate implementation portion of the study included logging onto CoPath to access the case being evaluated, followed by the multiple sequential steps of logging onto the hospital EHRs starting with Citrix XenApp and followed by EPIC. Once into EPIC reviewers must access patient station, typing and accepting the medical record number, followed by the navigation time required to fetch the relevant clinical, radiology, laboratory and anatomic pathology information. The time required for reviewing pathology slides and recording results in CoPath was then added.
The after implementation component of the study included the time required for the simultaneous logging onto the case in CoPath and Illuminate, the navigation of medical records in Illuminate, slide review and signing out in CoPath.
In addition, we studied the impact of implementing Illuminate on our transcriptionists’ workflow. Transcriptionists, following the dictation of gross findings, match the submitted surgical pathology requisitions accompanying specimens with working drafts of pathology reports including gross description and abbreviated versions of all previous surgical pathology and cytology diagnoses if available in our CoPath. Transcriptionists were asked to record the time involved in collecting the above information on a daily basis for two weeks prior to study implementation. Pathologists were able to access electronic versions of the draft report and all prior pathology material from Illuminate in its entirety.
Statistical analysis was performed using the Wilcoxon paired test. A p value of <0.05 was considered significant.
ResultsTop
Figures 1 and 2 showed schematic diagrams of the study comparing the pathologist's workflow before and after Illuminate implementation. Before Illuminate implementation the time required to retrieve any/all of the medical, radiological, pathology and laboratory records is illustrated (Figure 1). The components included in this portion are logging on the computer, CoPath, Citrix, O2 and EPIC, following by tabbing into the patient's records to locate relevant information and finally reviewing of the pathology slides and signing out the case in CoPath (Figure 1). In contrast, the after Illuminate implementation portion of the study included the time required for logging on to the computer, CoPath and Illuminate where the PatientView screen is populated automatically with patient's information in an itemized and categorized fashion (Figure 2). Figure 3a shows a screenshot illustrating the process where the pathologist is automatically directed to sign onto the Illuminate secure server after logging into CoPath. Once a pathologist opens a cytology or surgical pathology case on CoPath, Illuminate populates all available data from the medical records as shown in Figure 3b. Pathologists have access to all records itemized by reverse chronologic order, including clinical notes, radiology, clinical laboratory and anatomic pathology records. The system allows the users to navigate the records by filtering out irrelevant information using sub-second search capabilities. In particular, by simply hovering over a link (for clinical notes, radiology, clinical laboratory, or anatomic pathology reports) a synopsis of the report is seen. Subsequent clicking on the link opens an additional screen with the report to review in its entirety. Moreover, pathologists have the option to retrieve radiologic images in addition to reports by a link through Illuminate as shown in Figure 3c.
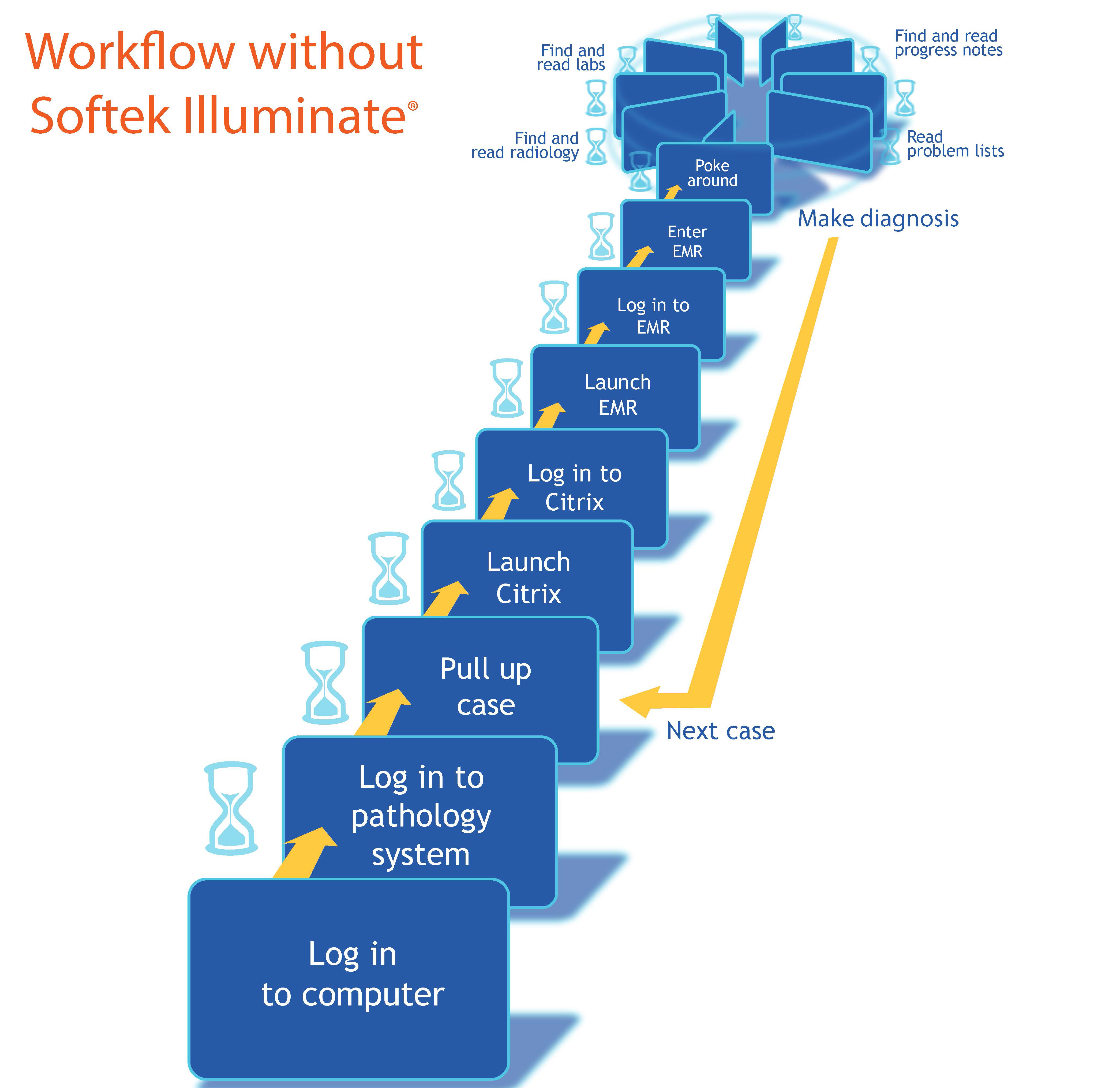
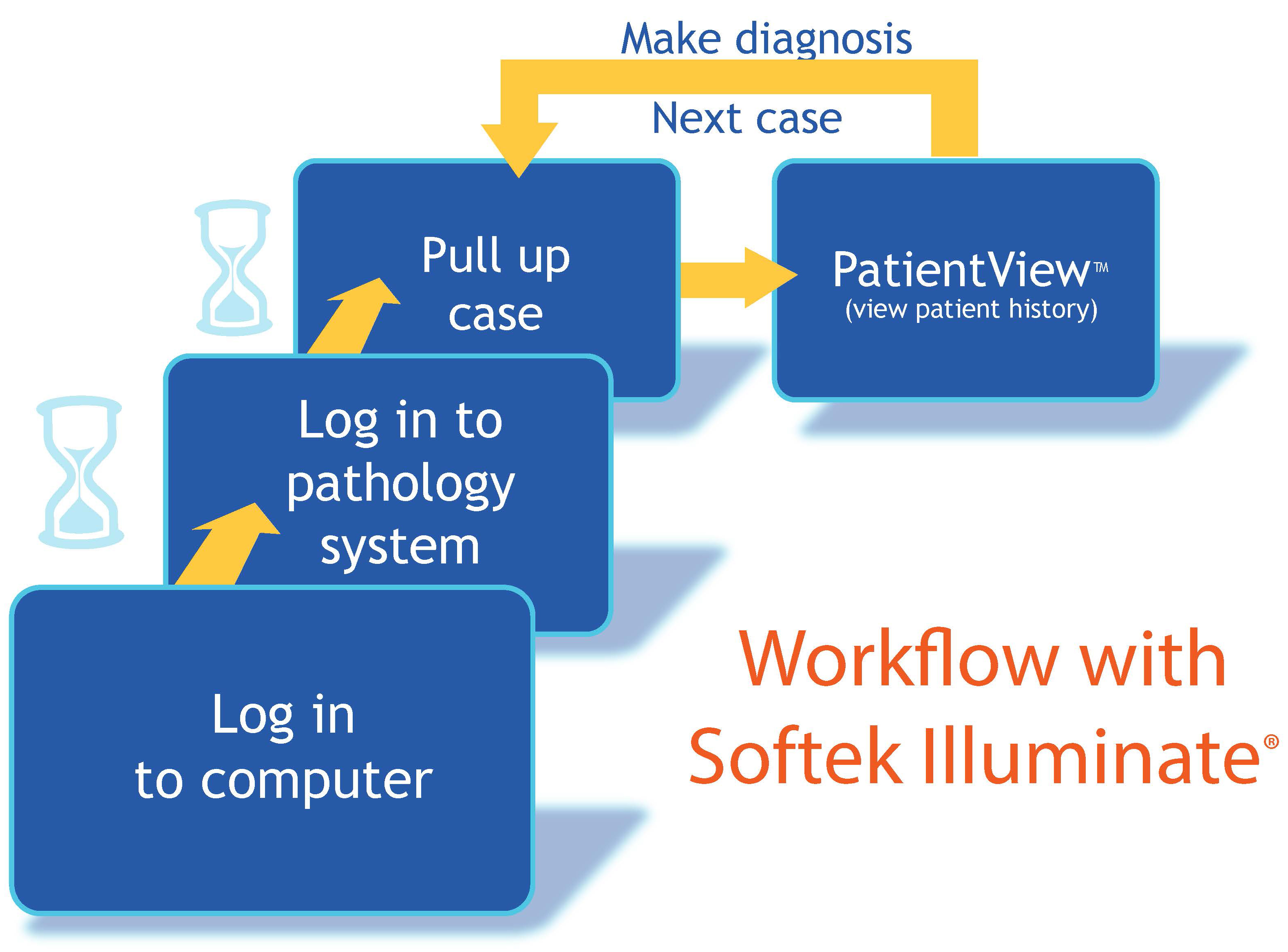
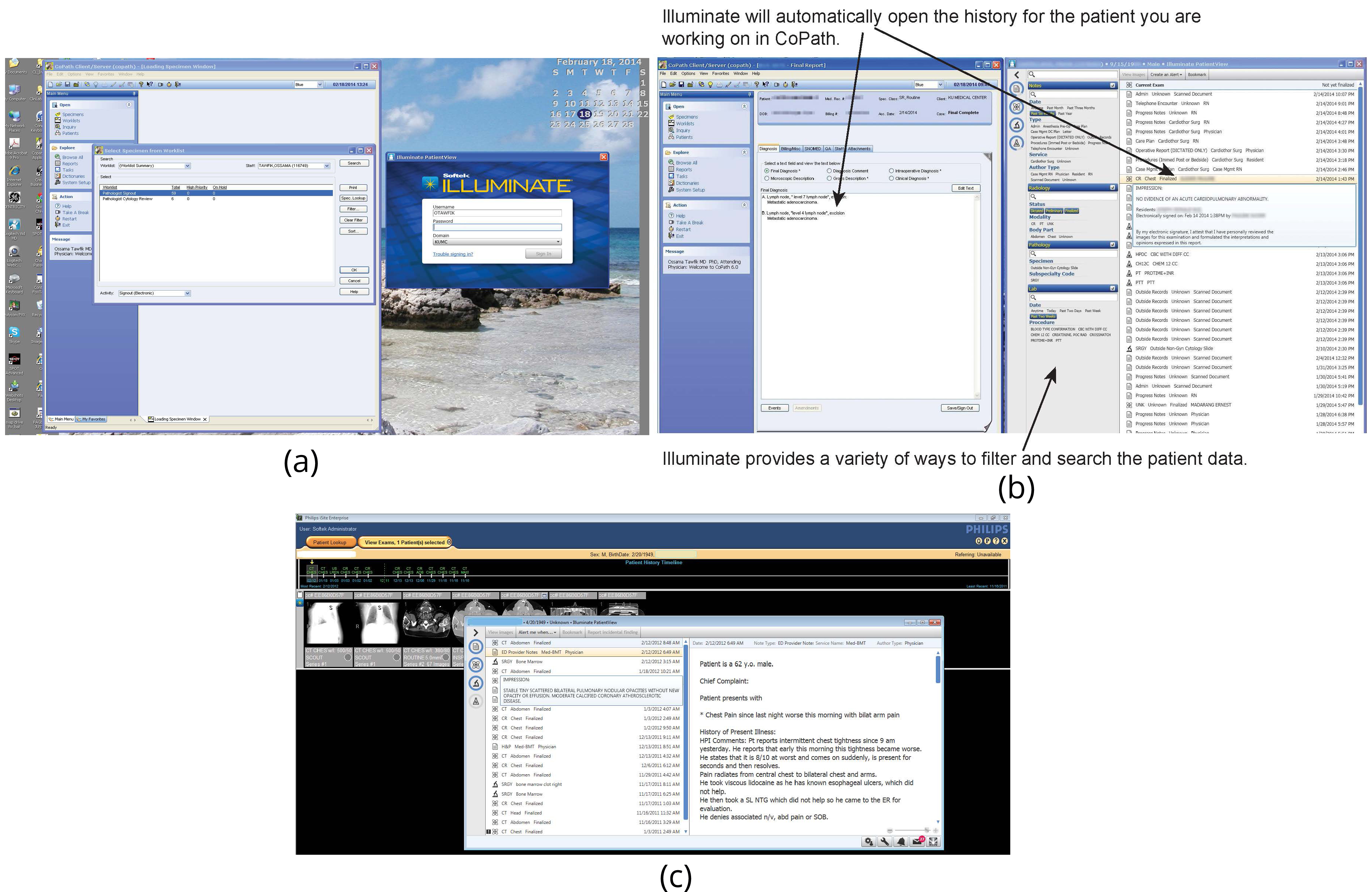
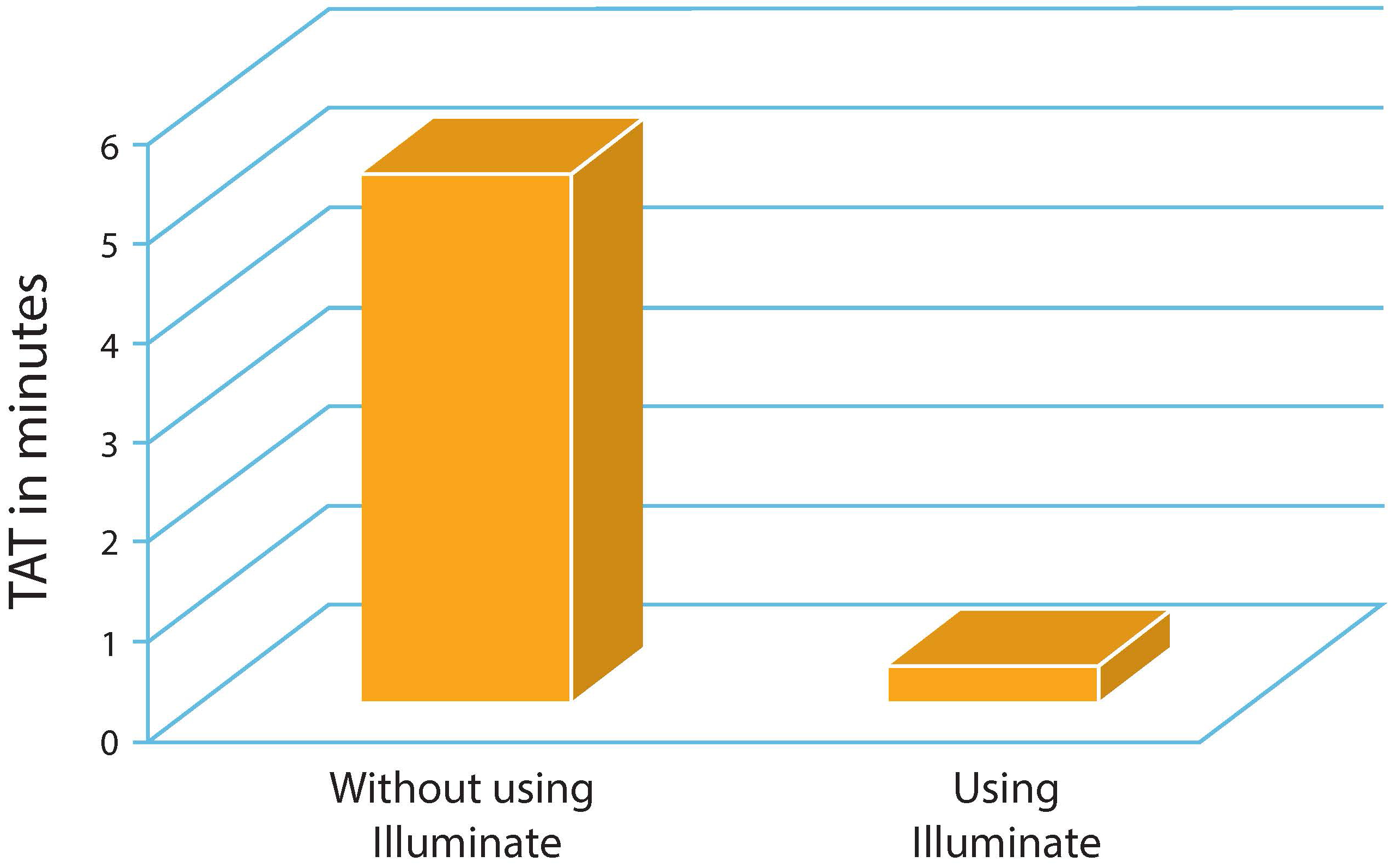
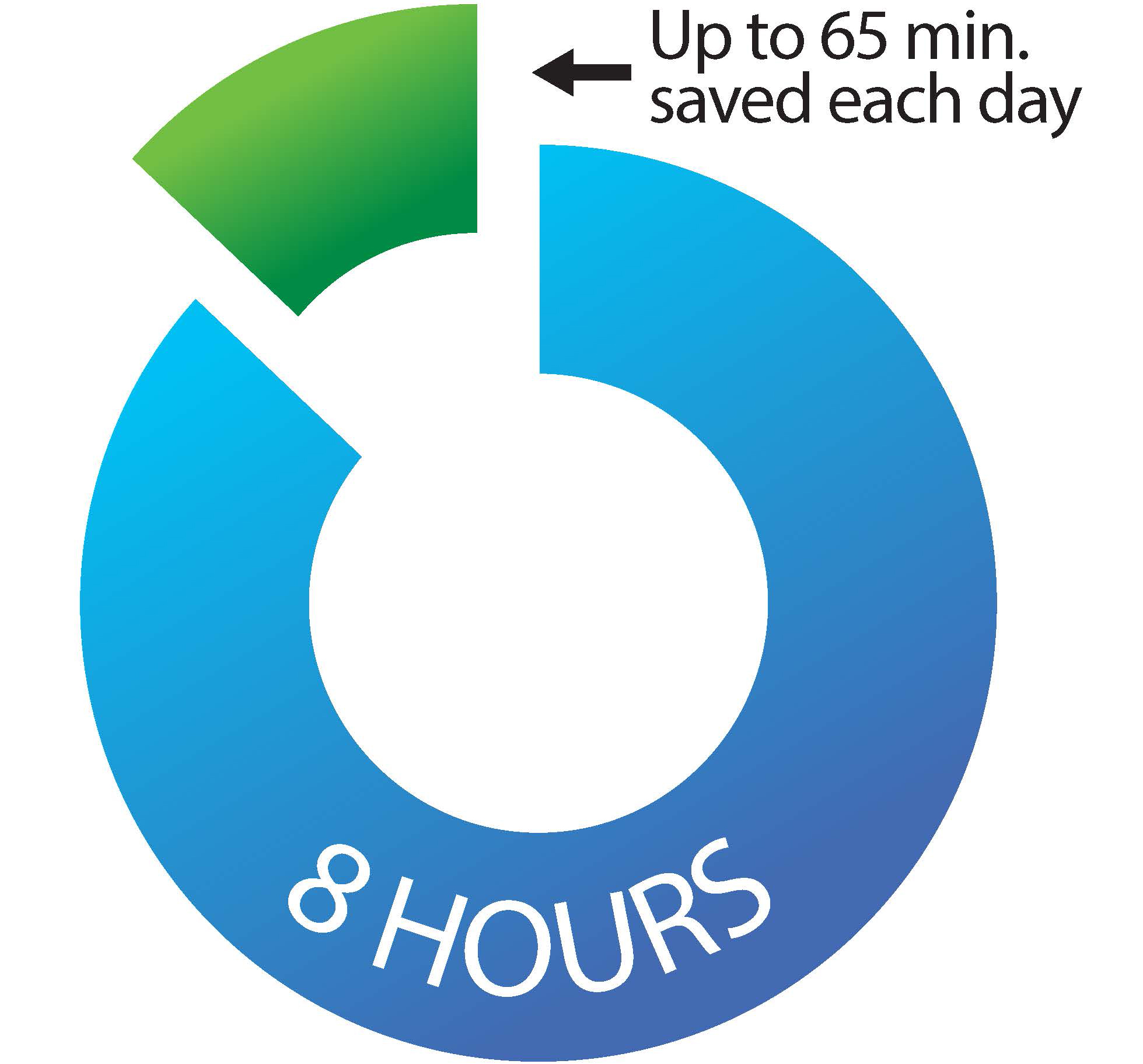
Figure 4 highlights the significant improvement in TAT by utilizing Illuminate. The average TAT/case of all pathologists retrieving various information prior to Illuminate implementation was 5:32 min (range 10:50 to 1:35 min; n = 200 cases). Post implementation time was significantly reduced to 35 seconds (range 10 sec to 1:10 min; n = 159 cases) (p value = <0.05). In addition, implementing Illuminate in the transcriptionists' workflow significantly improved their TAT and efficiency, eliminating up to 65 min/day (25-65 min) non-value added activity of matching requisitions with paperwork necessitated by a paper based workflow (Figure 5).
DiscussionTop
The Institute of Medicine released its landmark monograph “To Err is Human” in 1999 which has been the impetus for significant initiatives to improve patient safety. In its recent report it has identified medical errors as one of the most serious problems that lead to patients harm [10]. It encouraged physicians and other interested groups to work together to implement fixes to these problems. One of the most common problems is our inefficiency in extracting relevant clinical data in real time to try to prevent delay of patient care. The results of our study suggest that by incorporating interoperability software such as Illuminate's PatientView, in the pathologists' workflow we are able to improve pathologists' efficiency in signing out their cases by improved access to relevant clinical data.
Delay in patient care has been reported in up to 30% of hospitalized patients [11]. That delay has been in part attributed to scheduling of diagnostic tests, pending laboratory results and delays in medication administration [12]. Currently, significant time is wasted navigating EHRs for each patient and retrieving clinical, radiologic, laboratory and other previous pathology information. Thus new integrated information technology systems that facilitate the transmission of patient data could potentially improve the quality of care and reduce length of stay. Workflows in most pathology departments remain ad hoc to this day with multiple independent systems required to generate results for the current specimen and transmission to the rest of the healthcare enterprise. For example, even within the pathology department, anatomical and clinical pathology laboratories frequently use different information systems to track samples and to generate reports. In fact, not uncommonly laboratories may also use additional standalone systems to view and store pathology data such as gross images, digital images, outside consultation reports, or tests performed by an outside laboratory. Because all these data could be on the same patient, and therefore, essential to making correct diagnoses and directing patient management and treatment decisions, the isolation of this data causes unnecessary delays in the pathologists' workflows and ultimately patient care. These detrimental effects underscore the need for innovative workflow integration across multiple systems that facilitate the synthesis of data produced by the different specialties. Further improvements are required for full implementation of such systems into our daily routine. Studies are underway to integrate digital microscopic and gross images to patients' EHRs through Illuminate. Our hope is to provide all physicians the opportunity to access all pathology data remotely in real time at the time they wanted.
Pathologists, like radiologists, are physicians most often responsible for the initial diagnosis of complex diseases such as cancer. Collective information generated by these two specialists is vital for accurate diagnosis and staging with significant implications for the subsequent therapeutic options. Many studies have shown that integration of pathology-radiology workflows would improve overall outcomes of the diagnosis and treatment [13-18].
Radiologists using systems such as Illuminate were able to improve workflow, improve patient care, improve patient safety and cut costs [19-25]. This was primarily related to their improved ability in gathering information across hospital systems and providing instant access to relevant patient history and results of prior procedures to make better-informed decisions in less time.
Our study has validated the same concept in the world of pathology. We developed a comprehensive, user friendly integrated electronic patient summary to integrate the currently siloed subspecialty specific and EHRs systems. Users were successful in retrieving all up to date archived clinical, radiological, pathology and laboratory data in real time while logged onto their anatomic pathology systems without the need to log onto the main hospital electronic medical records system. Wasted time navigating EHRs for each patient and retrieving clinical, radiologic, laboratory and other previous pathology information was eliminated or substantially reduced. We were successful in executing a lean performance improvement concept to eliminate interruptions in workflow and thereby increase first time quality. The subsequent improvement in TAT should reduce delays in patient care, wasted resources and most importantly reduce potential harm. We were able to standardize the pathology report sign out process. The system has the capability of retrieving clinical notes in a variety of ways including clinical service, progress notes, care plan, operative notes, discharge summaries, procedures, author type, etc. Similarly radiology and laboratory information is retrievable by modality, date, procedure, body part and report status. In fact, retrievable information could be customized based on the needs of the pathologist and radiologist specific to their area of interest or expertise. Finally, utilizing such an approach has the potential of reducing cost or allowing resource reallocation. Based on our findings TAT for transcriptionists is estimated to be reduced by up to 20% of 1 full-time equivalent (FTE) and up to 15% for pathologists.
Despite findings consistent with improvement of TAT for pathologists and transcriptionists that incorporated Illuminate into their workflow, we noticed that full adoption of such systems in our workflow was a complex process that should be carefully planned and studied. The degree of satisfaction between individuals varies based on work habits. Some of pathologists expressed concerns in changing their sign out approach, suggesting that the outcome of adopting a productivity-enhancing technology can display variation based on individual habits and expectations. For example, some pathologists expressed concerns regards the lack of access to paper copies of previous pathology reports at the time of microscopic evaluation of their cases. This concern is despite the fact reports are available for review electronically on workstations in their entirety, unlike the abbreviated format currently presented in paper form. Others reported difficulty learning new technology or unsatisfaction due to alteration of the current workflow. Further improvements are required for full implementation of such systems into our daily routine. The current study has some limitation that should be pointed out. Although theoretically possible, integration with anatomic pathology systems other than Sunquest CoPath has not been tested. The study is also limited by the small number of samples and reviewers. Although promising, larger studies at multiple institutions are needed to validate and expand our pilot study.
ConclusionTop
An efficient interactive reporting system leads to real time interactions between ordering physicians, pathologists and radiologists, resulting in a tremendous impact on patient care.
Acknowledgments
Members of the department of Pathology and Laboratory Medicine at the University of Kansas Hospital would like to thank the leadership and staff of the Softek Solutions, Inc. for their commitment and support. Their vision in seeing the potential usefulness of such a concept and their willingness to share valuable company resources are tremendously appreciated.
Funding
This study is supported by internal institutional funds.
Conflicts of interest
All authors do not have potentially biasing relationship of a financial, professional or personal nature with any commercial interests that would constitute a conflict of interest related to the studies reported in this manuscript.
ReferencesTop
[1]Friedman BA. Informatics as a separate section within a department of pathology. Am J Clin Pathol. 1990; 94(Suppl 1):S2–6.Pubmed
[2]Buffone GJ, Beck JR. Informatics. A subspecialty in pathology. Am J Clin Pathol. 1993; 100(1):75–81.Article Pubmed
[3]Friedman BA, Martin JB. Hospital information systems. The physician's role. JAMA. 1987; 257(13):1792.Article Pubmed
[4]Korpman RA. Using the computer to optimize human performance in health care delivery. The pathologist as medical information specialist. Arch Pathol Lab Med. 1987; 111(7):637–645.Pubmed
[5]Hickner J, Thompson PJ, Wilkinsom T, Epner P, Sheehan M, et al. Primary care physicians’ challenges in ordering clinical laboratory tests and interpreting results. J Am Board Fam Med. 2014; 27(2):268–274.Article Pubmed
[6]Ahmed A, Chandra S, Herasevich V, Gajic O, Pickering BW. The effect of two different electronic health record user interfaces on intensive care provider task load, errors recognition, and performance. Cri Care Med. 2011; 39(7):1626–1634.Article Pubmed
[7]Boonn WW, Langlotz CP. Radiologist use of and perceived need for patient data access. J Digit Imaging. 2009; 22(4):357–362.Article Pubmed
[8]Bates DW, Gawande AA. Improving safety with information technology. N Eng J Med. 2003; 348(25):2526–2534.Article Pubmed
[9]Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc. 2011; 18(2):169–172.Article Pubmed
[10]Kohn LT, Corrigan JM, Donaldson MD, editors. To Err is human: Building a safer health system. Washington (DC): National Academies Press. 2000.Article Pubmed
[11]Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989; 27(2):112–129.Article Pubmed
[12]Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, et al. The timing of prophylactic administration of antibiotics and the risk of surgical wound infections. N Engl J Med. 1992; 326(5):337–339.Article Pubmed
[13]Tawfik O, Reddick M. Integrated radiology/pathology service for breast cancer. Critical Values. 2009; 2:23–26.Article
[14]Mihalik JE, Krupka L, Davenport R, Tucker L, Toevs C, et al. The rate of imaging-histologic discordance of benign breast disease: a multidisciplinary approach to the management of discordance at a large university-based hospital. Am J Surg. 2010; 199(9):319–323.Article Pubmed
[15]Travis W, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, et al. International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011; 6(2):244–285.Article Pubmed
[16]Galvin J, Frazier A, Franks T. Collaborative radiologic and histopathologic assessment of fibrotic lung disease. Radiology. 2010; 255(3):692–706.Article Pubmed
[17]Raghu G, Collard H, Egan J, Martinez FJ, Behr J, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011; 183(6):788–824.Article Pubmed
[18]Sorace J, Aberie DR, Elimam D, Lawvere S, Tawfik O, et al. Integrating pathology and radiology disciplines: an emerging opportunity? BMC Med. 2012; 10:100.Article Pubmed
[19]Nitrosi A, Bertolini M, Sghedoni R, Notari P, Pattacini P, et al. RIS-PACS, patient safety, and clinical risk management. Radiol Med. 2015; 120(6):498–503.Article Pubmed
[20]Harvey HB, Krishnaraj A, Alkasab TK. A software system to collect expert relevance ratings of medical record items for specific clinical tasks. JMIR Med Inform. 2014; 2(1):e3.Article Pubmed
[21]Langer SG, Tellis W, Carr C, Daly M, Erickson BJ, et al. The RSNA Image Sharing Network. J Digit Imaging. 2015; 28(1):53–61.Article Pubmed
[22]Medverd JR, Cross NM, Font F, Casertano A. Advanced medical imaging protocol workflow-a flexible electronic solution to optimize process efficiency, care quality and patient safety in the National VA Enterprise. J Digit Imaging. 2013; 26(4):643–650.Article Pubmed
[23]Yellowlees P, Odor A, Patrice K, Parish MB, Nafiz N, et al. Disruptive innovation: the future of healthcare? Telemed J E Health. 2011; 17(3):231–234.Article Pubmed
[24]Cowan IA, MacDonald SL, Floyd RA. Measuring and managing radiologist workload: measuring radiologist reporting times using data from a Radiology Information System. J Med Imaging Radiat Oncol. 2013; 57(5):558–566.Article Pubmed
[25]Chao ST, Meier T, Hugebeck B, Reddy CA, Godley A, et al. Workflow enhancement (WE) improves safety in radiation oncology: putting the WE and team together. Int J Radiat Oncol Biol Phys. 2014; 89(4):765–772.Article Pubmed



